Tag: health
A New Definition of the Nurse and Nursing as a Profession: What is a Nurse?

The International Council of Nurses (ICN) has released a new global definition of “nurse” and “nursing“, marking a significant milestone in the profession’s identity and global recognition.
Key Highlights:
- Purpose: The new definition aims to clearly articulate the scope, identity, and contribution of nursing to global health. It serves as a “global compass” for the profession.
- Core Values: It emphasizes nursing as a science-based, people-centered, and socially just profession, grounded in ethical standards and human connection.
- Development Process: The definition was the result of a year-long global initiative, involving an expert panel and a Delphi group of nurses from all ICN regions, ensuring cultural inclusivity and global consensus.
- Leadership and Support: ICN leaders, including CEO Howard Catton and Director David Stewart, highlighted the importance of defining nursing to ensure its visibility, value, and leadership in shaping health systems.
- Impact: The definition is intended to influence policy, education, regulation, and legal frameworks worldwide. It empowers nurses to fully embrace and lead within their roles.
This initiative is seen not just as a professional update, but as a reaffirmation of nursing’s leadership and identity for current and future generations
Warning of overseas outbreaks, CDC urges Americans to get the measles vaccine before traveling abroad
Story by Erika Edwards
With summer vacations quickly approaching, a serious and concerning new
The Centers for Disease Control and Prevention is urging Americans to make sure they’re protected against measles before traveling to other countries this summer.
Last week, the agency updated its travel guidance for the virus as cases pop up nationwide. Nearly all exposures at airports are linked to international travel.
That includes six cases linked to a Turkish Airlines flight that landed at Denver International Airport on May 13. The Colorado Department of Public Health and Environment said that four of the patients had been on the plane.
Warning of overseas outbreaks, CDC urges Americans to get the measles vaccine before traveling abroad
Two other people were exposed at the airport before getting sick. Measles is one of the most contagious viruses in the world. Droplets can linger in the air for up to two hours after an infected person has been there.
According to an NBC News tally, 1,125 measles cases in 33 states have been diagnosed in the U.S. this year. Texas, the state with the largest outbreak, has reported 738 cases.
The numbers are likely vast underestimates, experts say, because many people don’t get tested.
Three people, including two young girls in Texas, have died.
Canada and Mexico are also experiencing outbreaks. The Canadian government said it’s logged 2,515 confirmed or probable cases of measles since the beginning of the year.
Yemen, Pakistan and India top the CDC’s list of countries with the highest number of cases, but the agency notes that measles is a global problem.
“Measles outbreaks are happening in every region of the world. Anyone who is not protected against measles can get measles while abroad and easily spread it to others when they return home,” the CDC wrote on its website.
“Travelers can catch measles in many travel settings including travel hubs like airports and train stations, on public transportation like airplanes and trains, at tourist attractions, and at large, crowded events,” according to the agency’s latest guidance.
People traveling internationally who aren’t vaccinated or who have never had measles “should talk to their clinician and consider postponing their trip,” the agency said.
Babies as young as 6 months old can get an early dose of the measles-mumps-rubella vaccine at least two weeks before international travel, according to the CDC. Older kids and adults who don’t know whether they’ve been vaccinated should get two doses, 28 days apart before a trip.
It takes two weeks to build immunity. After that, people are considered 97% protected against measles infection.
This article was originally published on NBCNews.com
AACN Calls for Sustained Federal Investments in Nursing Education and the Workforce to Protect the Nation’s Health
 |
| AACN Calls for Sustained Federal Investments in Nursing Education and the Workforce to Protect the Nation’s Health WASHINGTON, D.C., June 3, 2025 – The American Association of Colleges of Nursing (AACN) strongly opposes reductions in federal funding for nursing education and research, which would weaken the nation’s healthcare workforce and reduce access to care. Supplementing the “skinny” budget issued in early May, the Trump Administration has released additional details about its fiscal year (FY) 2026 budget, which calls for significant cuts and the elimination of essential programs for academic nursing, which are currently administered by the Department of Health and Human Services (HHS) and Department of Education. Consistent with the reductions outlined in the President’s proposed budget, the Administration’s FY26 budget calls for the Health Resources and Services Administration (HRSA) to be reorganized into the Agency for a Healthy America, signaling reduced or eliminated funding for most of Title VIII Nursing Workforce Development Programs. Further, the budget proposes to eliminate the National Institute of Nursing Research (NINR) in addition to $18 billion in proposed cuts to the National Institutes of Health. Overall, the budget reduces HHS funding by roughly $31 billion. “The strength of America’s nursing workforce depends on consistent investment in programs that support pathways into nursing and lifesaving research,” said Dr. Deborah Trautman, President and Chief Executive Officer of AACN. “Eliminating or reducing this funding compromises our ability to prepare the next generation of nurses and ultimately threatens patient safety and care quality.” This budget also follows through on the President’s promise to dramatically reduce the footprint of the Department of Education with an overall reduction of $12 billion. “Academic nursing is the foundation of a resilient healthcare workforce,” said Dr. Jean Giddens, Chair of AACN’s Board of Directors. “Without a sustained commitment to higher education and the institutions that educate nurses of the future, we risk falling short in terms of workforce supply and stability.” AACN will continue to advocate vigorously for academic nursing and urge Congress to prioritize an FY 2026 budget that ensures support for our nation’s nurses. Funding Title VIII Nursing Workforce Development Programs and NINR are crucial investments in the healthcare infrastructure of our nation, directly contributing to the President’s goal of creating a healthy America.### The American Association of Colleges of Nursing (AACN) is the national voice for academic nursing representing more than 875 schools of nursing nationwide. AACN establishes quality standards for nursing education, influences the nursing profession to improve health care, and promotes public support of baccalaureate and graduate nursing education, research, and practice. |
| CONTACT: Robert Rosseter(202) 463-6930 ext. 231rrosseter@aacnnursing.org |
| American Association of Colleges of Nursing655 K Street NW, Suite 750Washington, DC 20001www.aacnnursing.org |
Charcot-Marie-Tooth (CMT)
Charcot-Marie-Tooth (CMT) disease is a group of inherited peripheral neuropathies affecting motor and sensory nerves. CMT can cause a a child to lose feeling and movement in their extremities. Sometimes this disease affects speech, breathing and swallowing. With this condition, the peripheral nerves (the nerves outside the brain and spinal cord) don’t work properly.



Pathophysiology
CMT results from mutations in genes involved in the structure and function of peripheral nerves. The pathophysiology varies depending on the specific type:
- Demyelinating forms (CMT1, CMT4, CMTX): Mutations affect Schwann cell function, leading to defective myelin production or maintenance. This results in reduced nerve conduction velocities.
- Axonal forms (CMT2): Mutations primarily affect axonal structure or function, leading to axonal degeneration.
- Intermediate forms: Show features of both demyelinating and axonal neuropathies.
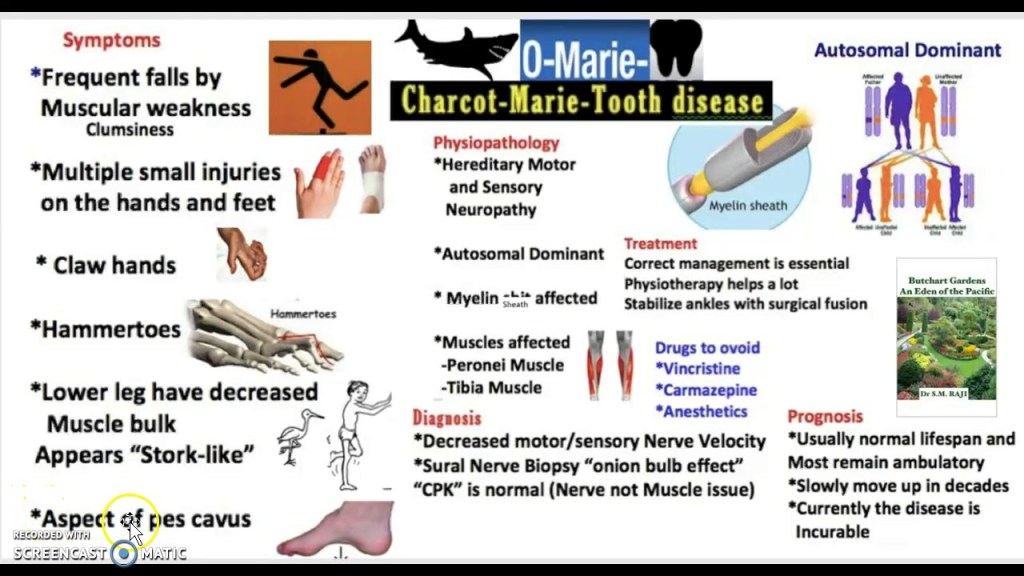
The common end result is progressive axonal loss, leading to muscle weakness and sensory deficits.
Genetic Transmission
CMT can be inherited in several patterns:
- Autosomal dominant: Most common in CMT1 and CMT2
- Autosomal recessive: Seen in some forms of CMT4
- X-linked: CMTX1 (mutations in GJB1 gene)
The most common mutations involve:
- PMP22 gene duplication (CMT1A)
- MPZ gene mutations (CMT1B)
- GJB1 gene mutations (CMTX1)
- MFN2 gene mutations (CMT2A)
X-linked CMT (CMTX) has a unique inheritance pattern compared to other forms of CMT
Inheritance through females
- When a female has X-linked CMT, each of her children (regardless of gender) has a 50% chance of inheriting the CMT-causing mutation.
- This is because females have two X chromosomes, and can pass either the affected or unaffected X chromosome to their children.
Inheritance through males
- When a male has X-linked CMT, all of his daughters will inherit the CMT-causing mutation.
- None of his sons will inherit the CMT-causing mutation.
- This is because males have one X and one Y chromosome. They always pass their X chromosome (which carries the mutation) to their daughters and their Y chromosome to their sons.
Key points
- X-linked CMT can be inherited through both males and females, but the pattern differs.
- Females can pass it to children of either gender.
- Males will only pass it to their daughters, not their sons.
- The inheritance pattern is different from autosomal dominant or recessive forms of CMT.
Severity
- Males with X-linked CMT typically have more severe symptoms than females.
- Females may have milder symptoms or be asymptomatic carriers due to having two X chromosomes (one normal, one with the mutation).
In summary, X-linked CMT can be inherited through both males and females, but the inheritance pattern and likelihood of passing on the condition differs based on the parent’s sex.



Signs and Symptoms
- Motor symptoms:
- Progressive distal muscle weakness and atrophy
- Foot deformities (pes cavus, hammer toes)
- Difficulty walking, frequent tripping
- Hand weakness and atrophy in later stages
- Sensory symptoms:
- Reduced sensation in feet and hands
- Neuropathic pain in some cases
- Other features:
- Reduced or absent deep tendon reflexes
- Scoliosis in some patients

Progression of CMT can be Quite Different for Different People
The progression of CMT syndrome can vary significantly between individuals, even within the same family. Here are some key points about how the progression can differ:
- Age of onset: Symptoms typically appear in adolescence or early adulthood, but can start anytime from early childhood to late adulthood. Some individuals may not realize they have CMT until later in life due to very mild symptoms.
- Rate of progression: CMT is generally slowly progressive, but the rate can vary. Some people experience rapid progression, while others have very slow progression over decades.
- Severity of symptoms: The severity ranges from mild cases with minimal impairment to severe cases causing significant disability. Most people fall in the moderate range.
- Distribution of symptoms: While CMT typically affects the feet and lower legs first, some individuals may experience hand and arm involvement earlier or more severely than others.
- Types of symptoms: The balance between motor and sensory symptoms can differ. Some people may have more muscle weakness, while others experience more sensory loss.
- Specific impairments: The development of foot deformities, hand dexterity issues, or breathing problems can vary widely between individuals.
- Impact on daily activities: The effect on walking, balance, fine motor skills, and overall quality of life differs for each person.
- Genetic factors: Different genetic mutations associated with CMT can lead to variations in disease progression and severity.
- Environmental factors: Lifestyle, overall health, and environmental factors may influence how the disease progresses in different individuals.
- Response to interventions: The effectiveness of treatments and interventions can vary between individuals, affecting the overall course of the disease.
It’s important to note that even within families carrying the same genetic mutation, there can be significant variability in how CMT progresses. Regular monitoring and personalized management are crucial due to this variability in progression.
Treatment Plans
There is no cure for CMT, so treatment focuses on symptom management and supportive care including physical therapy, occupational therapy, orthopedic interventions, pain management, genetic counseling for parents, and regular monitoring. Physical and occupational therapy might involve stretching and strengthening exercises, gait training, use of adaptive devices to improve hand and leg function, and strategies for regular activities of daily living (such as dressing, walking, grooming, toileting). Orthopedic interventions might include ankle-foot braces (also called ankle-foot orthoses or AFOs) for foot drop, or orthopedic surgery for deformities or scoliosis. Pain management can include over the counter pain medications, alternative pain therapy, or narcotics. Adults and parents of children with CMT can undergo genetic counseling. Finally, patients will be monitored for disease progression and deterioration.
References
- Aldihan, K. A., AlRashedi, M. J., Helayel, H. B., AlMutlak, M., & Hameed, S. T. (2023). Severe Dry Eye Disease in Charcot-Marie-Tooth Disease: A Comprehensive Case Report. American Journal of Case Reports, 24, 1–4. https://doi.org/10.12659/AJCR.941094
- Choi, J. E., Seol, H. Y., Seok, J. M., Hong, S. H., Choi, B. ‐O., & Moon, I. J. (2020). Psychoacoustics and neurophysiological auditory processing in patients with Charcot‐Marie‐Tooth disease types 1A and 2A. European Journal of Neurology, 27(10), 2079–2088. https://doi.org/10.1111/ene.14370
- Silsby, M., Yiannikas, C., Fois, A. F., Kennerson, M. L., Kiernan, M. C., Fung, V. S. C., & Vucic, S. (2024). Upper and lower limb tremor in Charcot-Marie-Tooth neuropathy type 1A and the implications for standing balance. Journal of Neurology, 271(4), 1776–1786. https://doi.org/10.1007/s00415-023-12124-z
- Waldman, L. E., Michalski, M. P., Pfeffer, G. B., Giaconi, J. C., & Learch, T. J. (2023). Charcot-Marie-Tooth Disease of the Foot and Ankle: Imaging Features and Pathophysiology. Radiographics, 43(4). https://doi.org/10.1148/rg.220114
Promoting Wellness in Nurses

Nurses play a pivotal role in the healthcare system, providing compassionate care and support to patients in diverse settings. However, the demands of the profession can take a toll on nurses’ physical, mental, and emotional well-being. Therefore, promoting wellness among nurses is not only essential for their individual health and job satisfaction but also crucial for maintaining high-quality patient care. Several strategies can be implemented to foster wellness in nurses.
First, creating a supportive work environment is paramount. Healthcare organizations should prioritize initiatives that prioritize the physical and psychological safety of nurses. Adequate staffing levels, manageable workloads, and supportive leadership contribute to a positive work environment where nurses feel valued and respected. Additionally, offering opportunities for professional development and career advancement empowers nurses and enhances their sense of fulfillment in their roles.
Second, promoting self-care practices is crucial for nurses’ wellness. Encouraging nurses to prioritize their physical health through regular exercise, proper nutrition, and sufficient sleep is essential for maintaining energy levels and resilience. Moreover, providing access to resources for stress management and relaxation techniques, such as mindfulness and meditation, equips nurses with coping mechanisms to navigate the challenges of their profession effectively.
Third, fostering a culture of open communication and peer support is instrumental in promoting wellness among nurses. Encouraging regular check-ins and debriefing sessions allows nurses to express their concerns, share experiences, and seek advice from colleagues. Peer support networks provide a sense of camaraderie and solidarity, fostering a supportive community where nurses can lean on each other for emotional support and encouragement.
Furthermore, implementing wellness programs tailored to nurses’ needs can significantly contribute to their overall well-being. These programs may include workshops on stress management, resilience-building activities, mental health awareness training, and access to counseling services. Providing nurses with resources and tools to prioritize their wellness empowers them to proactively manage their health and prevent burnout.
In conclusion, promoting wellness in nurses is essential for sustaining their health, job satisfaction, and ability to deliver high-quality patient care. By creating supportive work environments, promoting self-care practices, fostering peer support networks, and implementing wellness programs, healthcare organizations can invest in the well-being of their nursing staff. Ultimately, prioritizing nurses’ wellness not only benefits individual nurses but also enhances the overall resilience and effectiveness of the healthcare workforce.

Mastering Crucial Conversations: The Art of Effective Communication

In the realm of interpersonal dynamics, crucial conversations stand out as pivotal moments that can either propel relationships and projects forward or hinder progress and cause discord. Mastering the art of crucial conversations is essential in both personal and professional spheres. These conversations are characterized by high stakes, opposing opinions, and strong emotions, making them inherently challenging. However, when approached with intentionality, empathy, and effective communication strategies, they can lead to breakthroughs, understanding, and strengthened connections.
At the core of mastering crucial conversations lies the ability to cultivate a mindset of openness and curiosity. Rather than approaching these interactions defensively or with preconceived notions, individuals should strive to adopt a mindset of genuine inquiry and a willingness to understand different perspectives. This mindset shift sets the stage for constructive dialogue and fosters an environment where all parties feel heard and respected.
Active listening emerges as a cornerstone of effective communication during crucial conversations. It involves not only hearing the words spoken but also understanding the underlying emotions, concerns, and motivations. By attentively listening to both verbal and nonverbal cues, individuals can uncover the deeper meanings behind the discourse and respond in a manner that acknowledges these underlying sentiments. Furthermore, paraphrasing and summarizing what has been said can demonstrate genuine engagement and promote clarity, ensuring that all parties are on the same page.
Empathy plays a pivotal role in navigating crucial conversations with grace and understanding. Recognizing and validating the emotions of others can defuse tension and create an atmosphere of trust and collaboration. Empathetic responses convey that one values the other person’s perspective and experiences, even if they differ from one’s own. This validation fosters a sense of psychological safety, encouraging individuals to express themselves authentically without fear of judgment or reprisal.
Moreover, mastering crucial conversations entails the skillful management of emotions, both one’s own and those of others. Emotions often run high during these discussions, and unchecked emotional reactions can derail productive dialogue. By practicing emotional intelligence and self-regulation, individuals can navigate these intense feelings constructively, maintaining composure and rationality even in the face of adversity. Additionally, understanding the emotional triggers of others allows for more nuanced and empathetic responses, fostering mutual respect and understanding.
Finally, effective resolution strategies are crucial for bringing crucial conversations to a fruitful conclusion. Collaborative problem-solving techniques, such as exploring mutually beneficial solutions and seeking common ground, can bridge divides and lead to win-win outcomes. Additionally, a commitment to ongoing dialogue and follow-up ensures that agreements reached during the conversation are upheld and any lingering concerns are addressed promptly.
In conclusion, mastering crucial conversations is an essential skill set for navigating the complexities of interpersonal relationships and professional environments. By fostering a mindset of openness, practicing active listening and empathy, managing emotions effectively, and employing resolution strategies, individuals can transform potentially volatile discussions into opportunities for growth, understanding, and collaboration. Through intentional effort and continuous practice, one can harness the power of crucial conversations to cultivate stronger connections, drive positive change, and achieve shared goals.
References
Abadi S. (2021). Engaging in Crucial Conversations without Burning Bridges. The Canadian journal of hospital pharmacy, 74(2), 196.
Brouwer, M. A., Maeckelberghe, E. L. M., van der Heide, A., Hein, I. M., & Verhagen, E. A. A. E. (2021). Breaking bad news: what parents would like you to know. Archives of disease in childhood, 106(3), 276–281. https://doi.org/10.1136/archdischild-2019-318398
Freed, P. E., Frost, E., & Simmons, K. (2021). Crucial Conversations: Virtual Instruction, Sensitive Topics, and Safety in Groups. Nurse educator, 46(6), E143–E144. https://doi.org/10.1097/NNE.0000000000001087
Priftanji, D., Hill, J. D., & Ashby, D. M. (2020). Managing difficult conversations. American journal of health-system pharmacy : AJHP : official journal of the American Society of Health-System Pharmacists, 77(21), 1723–1726. https://doi.org/10.1093/ajhp/zxaa149
Promoting Wellness in Nurses

Nurses play a pivotal role in the healthcare system, providing compassionate care and support to patients in diverse settings. However, the demands of the profession can take a toll on nurses’ physical, mental, and emotional well-being. Therefore, promoting wellness among nurses is not only essential for their individual health and job satisfaction but also crucial for maintaining high-quality patient care. Several strategies can be implemented to foster wellness in nurses.
First, creating a supportive work environment is paramount. Healthcare organizations should prioritize initiatives that prioritize the physical and psychological safety of nurses. Adequate staffing levels, manageable workloads, and supportive leadership contribute to a positive work environment where nurses feel valued and respected. Additionally, offering opportunities for professional development and career advancement empowers nurses and enhances their sense of fulfillment in their roles.
Second, promoting self-care practices is crucial for nurses’ wellness. Encouraging nurses to prioritize their physical health through regular exercise, proper nutrition, and sufficient sleep is essential for maintaining energy levels and resilience. Moreover, providing access to resources for stress management and relaxation techniques, such as mindfulness and meditation, equips nurses with coping mechanisms to navigate the challenges of their profession effectively.
Third, fostering a culture of open communication and peer support is instrumental in promoting wellness among nurses. Encouraging regular check-ins and debriefing sessions allows nurses to express their concerns, share experiences, and seek advice from colleagues. Peer support networks provide a sense of camaraderie and solidarity, fostering a supportive community where nurses can lean on each other for emotional support and encouragement.
Furthermore, implementing wellness programs tailored to nurses’ needs can significantly contribute to their overall well-being. These programs may include workshops on stress management, resilience-building activities, mental health awareness training, and access to counseling services. Providing nurses with resources and tools to prioritize their wellness empowers them to proactively manage their health and prevent burnout.
In conclusion, promoting wellness in nurses is essential for sustaining their health, job satisfaction, and ability to deliver high-quality patient care. By creating supportive work environments, promoting self-care practices, fostering peer support networks, and implementing wellness programs, healthcare organizations can invest in the well-being of their nursing staff. Ultimately, prioritizing nurses’ wellness not only benefits individual nurses but also enhances the overall resilience and effectiveness of the healthcare workforce.

Summary of Article “Dementia, Driving, and the Duty to Warn”
The article discusses the relationship between mandatory reporting of dementia to vehicle licensing agencies and the potential underdiagnosis of dementia by physicians. Here are the key points:

- A study by Jun et al. conducted a cross-sectional ecological analysis of four states with mandatory fitness-to-drive reporting of dementia.
- The results suggest that mandatory reporting is associated with an increase in physicians underdiagnosing dementia:
- 12.4% in states with mandatory reporting
- 7.8% in states with driver self-reporting
- 7.7% in states with no mandates
- The implication is that mandatory reporting may be aversive to patients and clinicians, leading to widespread underdiagnosis.
- The article cautions against drawing causal conclusions from this correlation, as there could be other factors influencing the results.
- The tension between patient privacy and community safety in relation to dementia and driving is highlighted as a complex issue.
- The importance of counseling patients about road safety is emphasized, regardless of government mandates.
- The article notes that while mandatory reporting may have unintended consequences, it’s essential for clinicians to address driving safety with dementia patients.
- The authors suggest that tactful counseling, focusing on practical alternatives and treating comorbidities, is crucial when discussing driving limitations with dementia patients.
The article ultimately emphasizes the need for a balanced approach to addressing dementia and driving safety, considering both patient care and public safety concerns.
Redelmeier DA, Bhatt V. Dementia, Driving, and the Duty to Warn. JAMA Netw Open. 2024;7(4):e248856. doi:10.1001/jamanetworkopen.2024.8856

Leave a comment