Essential hypertension, also known as primary hypertension, is a chronic medical condition characterized by persistently elevated blood pressure without an identifiable underlying cause. It is the most common form of hypertension, accounting for about 90-95% of all cases of high blood pressure.
Prevalence and Incidence in the US
According to the Centers for Disease Control and Prevention (CDC), nearly half of adults in the United States (47%, or 116 million) have hypertension. The prevalence of hypertension increases with age, affecting about 63% of adults aged 60 and older. The incidence of newly diagnosed hypertension is estimated to be about 2.5% per year among adults in the US.
Epidemiology
Several factors contribute to the epidemiology of essential hypertension:
- Age: The risk increases with age, with a sharp rise after 65 years.
- Gender: Men are at higher risk until age 65, after which women’s risk surpasses that of men.
- Race: African Americans have a higher prevalence and earlier onset compared to other racial groups.
- Family history: There is a strong genetic component to essential hypertension.
- Lifestyle factors: Obesity, physical inactivity, high salt intake, and excessive alcohol consumption increase risk.
Pathophysiology
The exact pathophysiology of essential hypertension is complex and not fully understood. It involves multiple interacting factors:
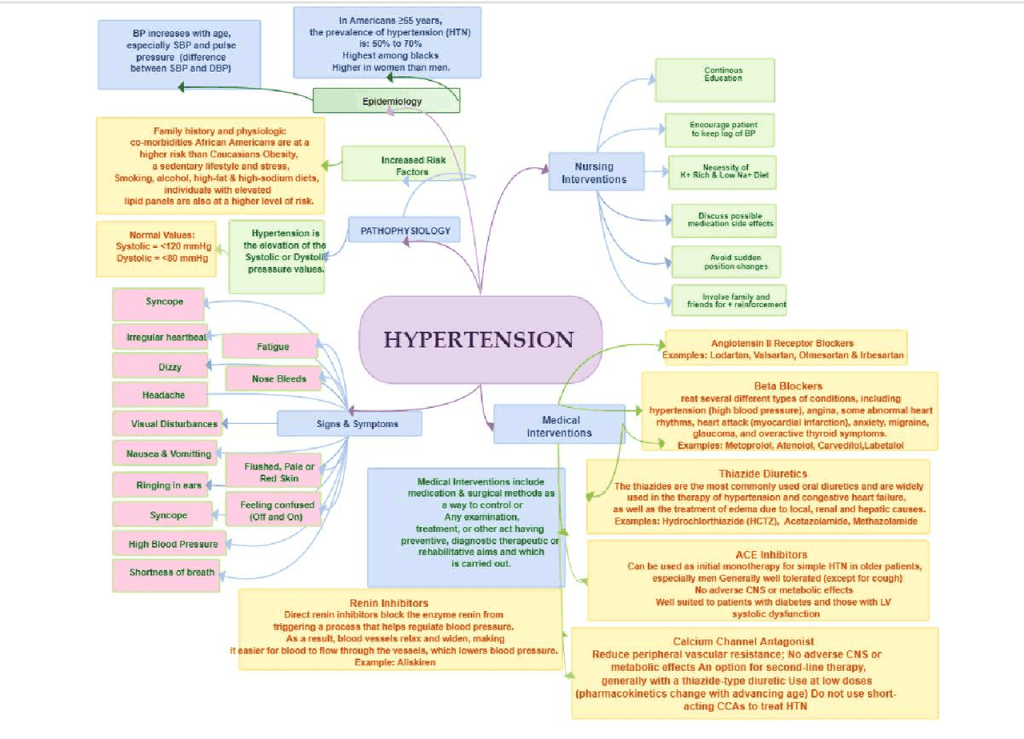
Increased sympathetic nervous system activity
Overactivation of the renin-angiotensin-aldosterone system (RAAS)
Endothelial dysfunction leading to increased vascular resistance
Impaired sodium excretion by the kidneys
Genetic factors influencing salt sensitivity and vascular reactivity
Inflammation and oxidative stress
These factors interact to cause increased peripheral vascular resistance and/or increased cardiac output, leading to elevated blood pressure.
Signs and Symptoms
Essential hypertension is often called the “silent killer” because it typically has no symptoms in its early stages. Most people with hypertension feel normal. However, some individuals may experience:
- Headaches, particularly in the morning
- Dizziness
- Blurred vision
- Nosebleeds
- Shortness of breath
- Chest pain
It’s important to note that these symptoms usually occur only when blood pressure reaches dangerously high levels or in cases of hypertensive crisis.
Complications
If left untreated, essential hypertension can lead to serious complications:
- Heart disease (coronary artery disease, heart failure)
- Stroke
- Kidney damage
- Vision problems
- Peripheral artery disease
Diagnosis
Diagnosis is made through consistent blood pressure measurements over time. According to current guidelines:
- Normal: Less than 120/80 mm Hg
- Elevated: 120-129/less than 80 mm Hg
- Stage 1 hypertension: 130-139/80-89 mm Hg
- Stage 2 hypertension: 140/90 mm Hg or higher
Treatment
Management of essential hypertension involves both lifestyle modifications and pharmacological interventions:
- Lifestyle changes: Weight loss, regular exercise, reducing salt intake, limiting alcohol, and adopting a heart-healthy diet (like DASH diet).
- Medications: Including ACE inhibitors, ARBs, calcium channel blockers, diuretics, and beta-blockers.
Conclusion
Essential hypertension is a widespread condition with significant health implications. While it often has no symptoms, its potential for serious complications makes regular blood pressure monitoring crucial. With proper management through lifestyle changes and medication when necessary, most people with essential hypertension can effectively control their blood pressure and reduce their risk of complications.
References
- Unger T, Borghi C, Charchar F, et al. 2020 International Society of Hypertension Global Hypertension Practice Guidelines. Hypertension. 2020;75(6):1334-1357. doi:10.1161/HYPERTENSIONAHA.120.15026
- Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71(6):e13-e115. doi:10.1161/HYP.0000000000000065
- Williams B, Mancia G, Spiering W, et al. 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J. 2018;39(33):3021-3104. doi:10.1093/eurheartj/ehy339
- Muntner P, Shimbo D, Carey RM, et al. Measurement of Blood Pressure in Humans: A Scientific Statement From the American Heart Association. Hypertension. 2019;73(5):e35-e66. doi:10.1161/HYP.0000000000000087
- Carey RM, Calhoun DA, Bakris GL, et al. Resistant Hypertension: Detection, Evaluation, and Management: A Scientific Statement From the American Heart Association. Hypertension. 2018;72(5):e53-e90. doi:10.1161/HYP.0000000000000084
- Arnett DK, Blumenthal RS, Albert MA, et al. 2019 ACC/AHA Guideline on the Primary Prevention of Cardiovascular Disease: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;140(11):e596-e646. doi:10.1161/CIR.0000000000000678
- Flack JM, Adekola B. Blood pressure and the new ACC/AHA hypertension guidelines. Trends Cardiovasc Med. 2020;30(3):160-164. doi:10.1016/j.tcm.2019.05.003
- Burnier M, Bakris G, Williams B. Redefining diuretics use in hypertension: why select a thiazide-like diuretic? J Hypertens. 2019;37(8):1574-1586. doi:10.1097/HJH.0000000000002088
- Drawz PE, Ix JH. BP Measurement in Clinical Practice: Time to SPRINT to Guideline-Recommended Protocols. J Am Soc Nephrol. 2018;29(2):383-388. doi:10.1681/ASN.2017070818
- Egan BM, Stevens-Fabry S. Prehypertension–prevalence, health risks, and management strategies. Nat Rev Cardiol. 2015;12(5):289-300. doi:10.1038/nrcardio.2015.17