COPD is a significant global health burden, with a growing prevalence and substantial impact on morbidity and mortality. The pathophysiology of COPD involves complex interactions between genetic predisposition, environmental factors, and inflammatory processes. This manuscript aims to elucidate the intricate mechanisms that contribute to the development and progression of COPD, providing insights into potential therapeutic targets and strategies.
COPD
- Risk Factors and Etiology: COPD is predominantly associated with cigarette smoking, which accounts for the majority of cases. Other risk factors include exposure to biomass fuel smoke, occupational dust and chemicals, genetic predisposition, and respiratory infections during childhood. The interplay between these risk factors and individual susceptibility determines the likelihood of developing COPD.
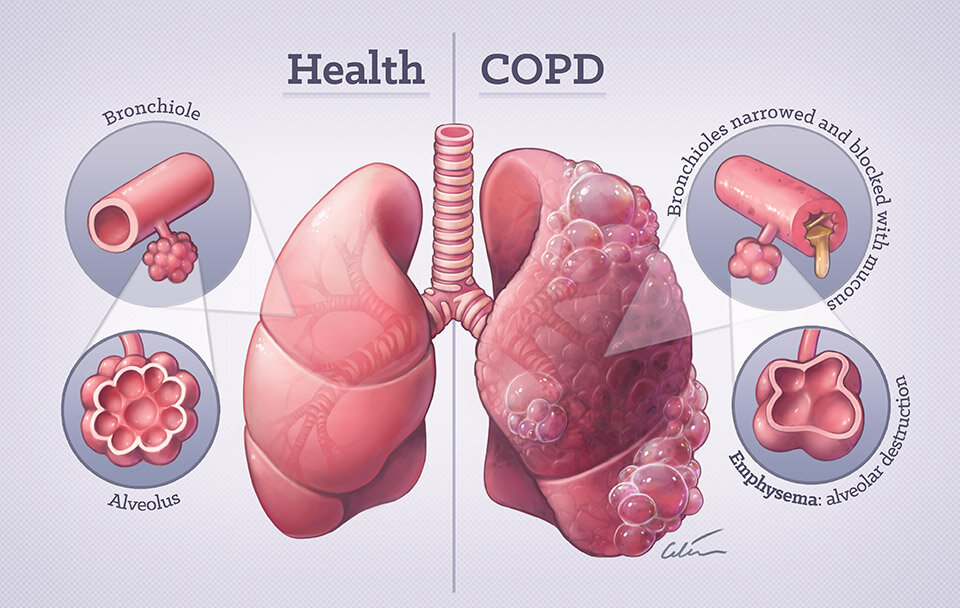
- Airway Inflammation and Remodeling: Central to the pathophysiology of COPD is chronic inflammation within the airways and lung parenchyma. Inhalation of noxious particles and gases, particularly cigarette smoke, triggers an immune response characterized by the recruitment and activation of inflammatory cells, such as neutrophils, macrophages, and T lymphocytes. These inflammatory cells release various mediators, including cytokines, chemokines, and proteases, leading to tissue damage, airway remodeling, and mucus hypersecretion.
- Oxidative Stress and Antioxidant Imbalance: COPD is associated with increased oxidative stress, resulting from an imbalance between the production of reactive oxygen species (ROS) and the antioxidant defense mechanisms. Cigarette smoke is a major source of ROS, which can cause direct damage to cellular components, including lipids, proteins, and DNA. Furthermore, ROS can activate inflammatory pathways and contribute to the pathogenesis of COPD.
- Protease-Antiprotease Imbalance: A critical feature of COPD is the disruption of the protease-antiprotease balance within the lung tissue. Proteases, such as matrix metalloproteinases (MMPs) and neutrophil elastase, are involved in tissue remodeling and degradation of extracellular matrix components. In COPD, there is a relative deficiency of antiproteases, such as alpha-1 antitrypsin, leading to uncontrolled protease activity and destruction of lung parenchyma.
- Small Airway Disease and Emphysema: Structural changes in the small airways and alveolar tissue contribute to airflow limitation in COPD. Small airway disease is characterized by inflammation, fibrosis, and luminal narrowing, leading to increased airway resistance and decreased airflow. Emphysema, on the other hand, involves the destruction of alveolar walls and loss of lung elasticity, resulting in airspace enlargement and impaired gas exchange.
- Pulmonary Vascular Changes: COPD is associated with pulmonary vascular remodeling and endothelial dysfunction, which contribute to pulmonary hypertension and right heart failure. Hypoxia-induced vasoconstriction, inflammation-mediated endothelial injury, and imbalance of vasoactive mediators contribute to pulmonary vascular changes in COPD.
Conclusion: In summary, COPD is a multifactorial disease characterized by chronic inflammation, oxidative stress, protease-antiprotease imbalance, and structural changes within the respiratory system. A comprehensive understanding of the pathophysiological mechanisms underlying COPD is essential for developing targeted therapies and improving clinical outcomes for patients with this debilitating condition. Further research is needed to elucidate additional contributors to COPD pathogenesis and identify novel therapeutic approaches.